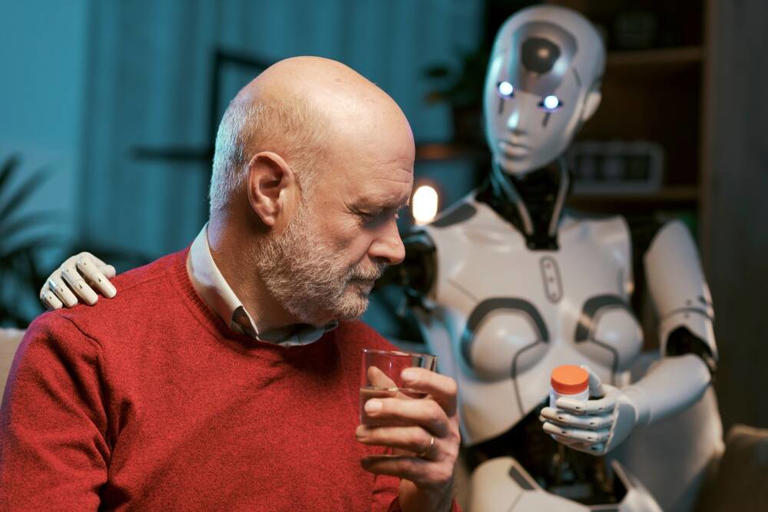
AI is used everywhere. We interact with Chat Bots at least once a week. We expect the Bot to be correct and believe the information we are given. This article puts a focus on the responsibility of an organization to ensure the information being provided by the BOT is correct. The area of health care is particularly disconcerting as the risk of death could be high.
Governments are beginning to realize the risk of using AI and are putting policies and regulations in place to reduce the risks of using AI. It is a matter a time before companies will be held accountable for the use of AI. A new ISO standard has just been released to provide a guideline for the management of the creation and use of AI -ISO 42001. It is a matter of time before certification to ISO 42001 will be mandated.
Story by Thomas Claburn – The Register
UnitedHealthcare has been sued for allegedly denying healthcare claims based on a faulty AI model.…
The lawsuit [PDF], filed Tuesday in federal court in Minneapolis on behalf of the estates of two elderly men, alleges that at least since UnitedHealthcare’s 2020 acquisition of post-acute care management firm Navihealth, the US health insurance giant has repeatedly and wrongfully refused to pay the healthcare claims of senior patients using their Medicare Advantage Plans, apparently using advice from a self-serving algorithm.
UnitedHealthcare is quite large: it was ranked 10th in the Fortune Global 500 this year and serves about 46 million people in the United States alone.
Medicare Advantage is a privately-run, government-approved version of the federal Medicare program and provides health coverage for US citizens or residents who are age 65 or older. Presently, approximately 31 million people in the US rely on Medicare Advantage.
Various studies suggest both Medicare and Medicare Advantage have attractive points for certain health issues, though an April 2022 report [PDF] from the Inspector General of the US Department of Health and Human Services found that private Medicare Advantage programs deny 13 percent of service authorization requests that would have been approved by government-run Medicare.
The complaint, brought by Clarkson Law Firm, alleges UnitedHealthcare unlawfully deployed an AI system with a 90 percent error rate that improperly overrode the recommendations of physicians regarding medically necessary post-acute care for the elderly, i.e. treatment following discharge from a hospital.
“UnitedHealthcare is responsible for the health care needs of some of our most vulnerable populations,” said Ryan Clarkson, managing partner of Clarkson Law, in a statement. “But by invoking this technology, they are effectively using AI to throw the elderly – our parents or grandparents – out onto the street.”
The nH Predict AI Model allegedly produces generic care recommendations that fail to account for the individual needs of patients, and also conflicts with Medicare Advantage coverage rules while conveniently saving UnitedHealthcare money. And it’s claimed that UnitedHealthcare has instructed its employees not to deviate from its AI model’s predictions about appropriate care and that the medical biz disciplines or terminates those who do so.
“Under Medicare Advantage Plans, patients who have a three-day hospital stay are typically entitled to up to 100 days in a nursing home,” the lawsuit claimed, citing an investigative report from medical publication STAT earlier this year.
“With the use of the nH Predict AI Model, [UnitedHealthcare] cut off payment in a fraction of that time. Patients rarely stay in a nursing home more than 14 days before they start receiving payment denials.”
The complaint stated that when patient claim denials are appealed internally or via a federal Administrative Law Judge, 90 percent of the nH Predict determinations are reversed.
“This demonstrates the blatant inaccuracy of the nH Predict AI Model, and the lack of human review involved in the coverage denial process,” the lawsuit claimed, adding that nH Predict determinations are not communicated to patients’ doctors and that when inquiries are made, UnitedHealthcare employees deny their requests and claim the decision information is proprietary.
Our ISO 42001 Implementer training 5-day self-study is here to assist companies during their implementation of an AI Management System based on ISO 42001. With new requirements in Europe driving companies towards certification, be the first to implement ISO 42001 and become certified.
Our PECB published course is designed to assist you in this endeavor. Contact me at training@cpisys for more information and get started on your AI certification journey!